Clinical Pathology Laboratories will work with ordering clinicians and their patients to obtain the required prior authorization based upon the requirements established by each payor.
When a test is ordered that is deemed as a molecular or genetic test, the laboratory will contact the payor to inquire about what is required. Clinical information and patient history may be requested for submission to the payor to determine medical necessity and coverage criteria. Once a denial or authorization is obtained, the laboratory will contact the provider and/or patient to inform them of the outcome and to educate them regarding their options for testing and financial responsibility.
Important Note: Prior authorization approvals are coverage determinations and do not eliminate the patient’s financial responsibility, if applicable.
Prior Authorization FAQs
How can I determine coverage for specific services as well as my financial responsibility?
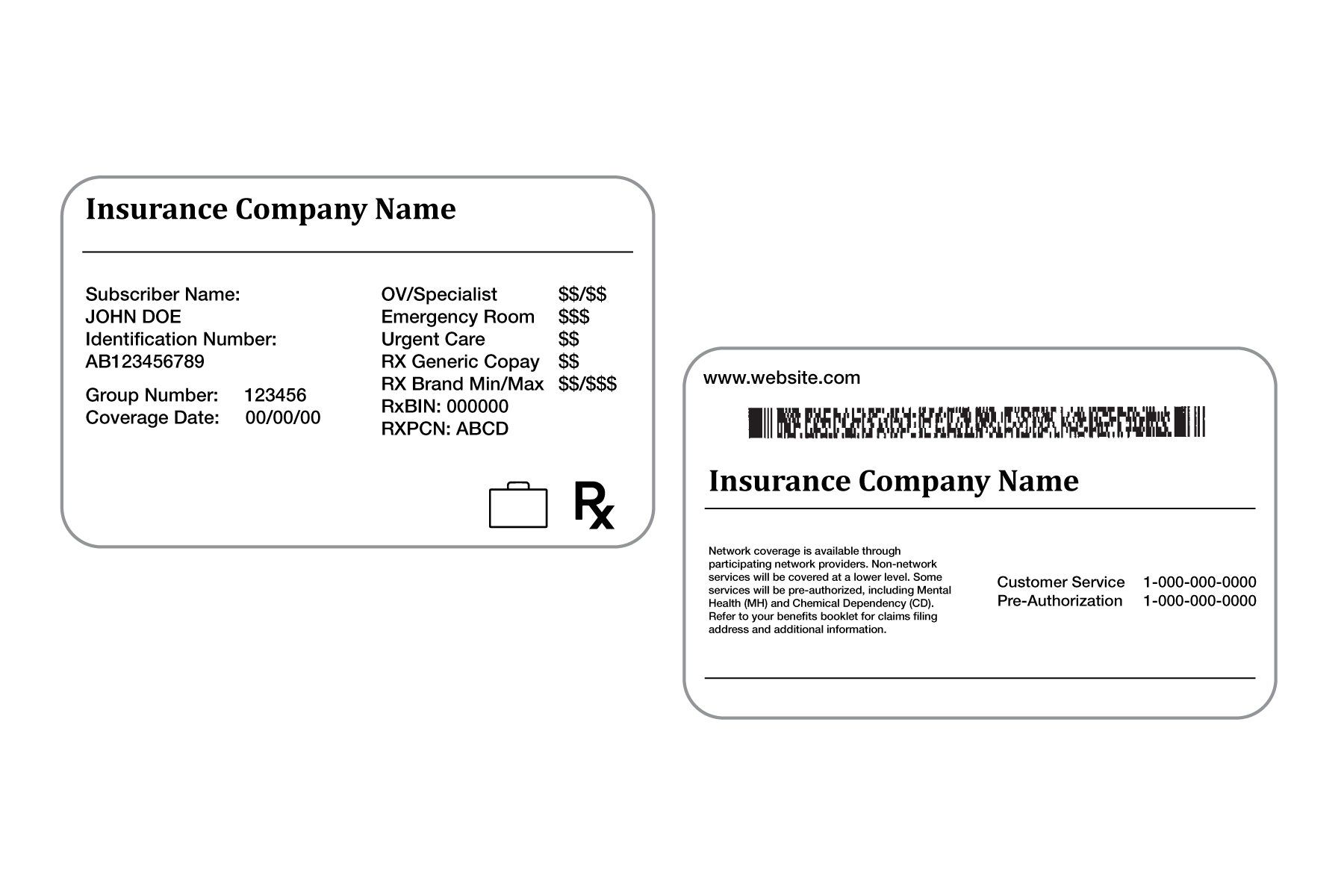
You may have received a card or other document as proof of health insurance. All cards vary, but should have the same type of information as the example shown below.
Contact your insurance company’s Member Services or Customer Service department for help in determining coverage for specific services as well as your financial responsibility. Some important questions to ask:
- Are these CPT and/or ICD-10 codes covered under my policy?
- CPT codes (also called the procedure codes) will be provided by CPL
- ICD-10 codes (also called the diagnosis codes) will be provided by your physician
- What is my out-of-pocket financial responsibility for these CPT and/or ICD-10 codes, including deductible or copay?
- What medical criteria must be met?
- Does this test require prior authorization?
How is prior authorization obtained?
The Member Services or Customer Service department at your insurance company should be able to provide you with specific requirements for your policy. Upon receipt of your lab orders and sample, CPL will contact your insurance company to verify eligibility and benefits along with prior authorization requirements. CPL will coordinate with your physician for submission of the necessary documentation to your insurance company to request a prior authorization review. After the prior authorization case is approved by your insurance company, testing can begin.
What do I do if the prior authorization for my test is denied or the test is not a covered benefit under my policy?
Even if prior authorization for your test is denied or your insurance policy excludes the service from benefits, you may still seek testing but you will be held responsible for the cost of the test(s). CPL offers a patient savings program or financial assistance for patients who meet criteria. Please reach out to a CPL Care Specialist at 833.583.2028 for more information on these programs or assistance with the prior authorization process. We are available Monday-Friday, 8AM to 5PM central time, closed Noon to 1PM for lunch.

